Many patients come to us wanting to understand the difference between gingivitis vs periodontitis. Both are forms of gum disease, but they do not affect the mouth in the same way or cause the same level of damage. Knowing how these conditions differ is a key step in maintaining strong, healthy gums. We focus on early recognition and preventive treatments so gum disease can be managed before it becomes more serious.
Gingivitis vs periodontitis: What these conditions mean
What is gingivitis?
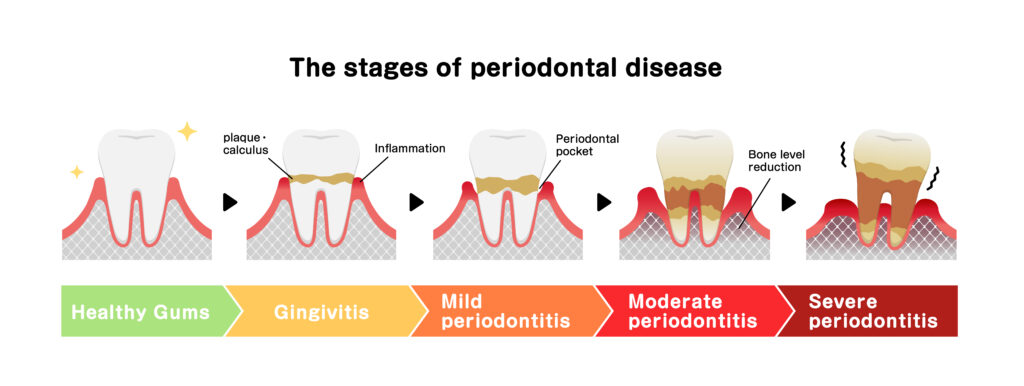
Gingivitis is the early stage of gum disease. It begins when plaque is left along the gumline and irritates the gum tissue. At this point, the gums may look red, swollen, or may bleed easily, especially when you brush your teeth or floss. Gingivitis affects the surface level of the gums and does not involve bone loss. The good news is that gingivitis can often be fully reversed with good oral hygiene and a professional cleaning that removes tartar and bacteria.

What is periodontitis?
Periodontitis is a more serious form of periodontal disease. Instead of affecting only the surface tissues, periodontitis begins to damage the ligaments and bone that support the teeth. As the infection progresses, deep pockets can form around the teeth, and the gums may start to pull away, leading to gum recession. Left untreated, this stage of gum disease can lead to mobility issues and even tooth loss. Periodontitis cannot be reversed, but it can be controlled with the right periodontitis treatment and consistent follow-up care.
Gingivitis vs periodontitis: Key differences you should know
Inflammation vs bone loss
The main difference between gingivitis and periodontitis is how deeply the inflammation has spread. Gingivitis affects only the gums. Periodontitis involves the gums, the ligaments, and the bone that hold the teeth in place. Once the bone is affected, this becomes a more advanced condition.
Reversibility vs permanent damage
Gingivitis is usually reversible with improved home care and a dental cleaning that removes tartar and plaque. Periodontitis causes permanent structural changes because bone does not grow back once it has been lost. We can treat and manage periodontitis, but we cannot undo the bone damage that has already occurred.
When gingivitis progresses into periodontitis
Untreated gingivitis can eventually advance into periodontitis, especially if plaque and tartar remain along the gums. Over time, the body responds to the bacteria by breaking down surrounding tissues. When that happens, the condition moves from an early-stage problem into an advanced gum disease that requires deeper treatment.
Signs of gingivitis and early gum inflammation
How gingivitis starts
Gingivitis begins when plaque stays on the teeth and gums for too long. Without consistent brushing and flossing, plaque hardens into tartar, which cannot be removed at home. This buildup irritates the gums and triggers inflammation. If we identify gingivitis early, the treatment is generally simple and very effective.
Symptoms that show your gums are irritated
Common signs of gingivitis include:
- bleeding gums during brushing or flossing
- gums that appear red or puffy
- mild tenderness along the gumline
- bad breath that does not improve with brushing
These symptoms are signals that the gums need attention and improved care. Catching gingivitis early not only protects the gums but also prevents the condition from progressing into something more difficult to manage.
How to know if you have periodontitis
Symptoms of advanced gum disease
Periodontitis has a different set of symptoms than gingivitis. Since the infection reaches deeper tissues, the signs tend to be more noticeable. These may include:
- ongoing bad breath
- deep pockets between the teeth and gums
- gums pulling away or shrinking
- discomfort when chewing
- changes in how the teeth fit together
These symptoms of periodontitis indicate that the gums and supporting bone have begun to break down.
Warning signs of bone loss and deep pockets
Bone loss often develops quietly, so patients may not realize it is happening. Pockets deeper than normal can form around the teeth, trapping bacteria and making it harder to maintain good oral hygiene. As the condition progresses, teeth may start to loosen. Recognizing these signs early allows us to begin periodontitis treatment before more damage occurs.
Types of periodontitis diagnosed by dentists
Periodontitis
This is the most common form of periodontal disease. We now classify it by stages and grades, which describe how much damage is present and how quickly the condition is progressing. Some people experience what we refer to as slow progression, where bone loss and gum recession develop gradually over time. Others may have a type that causes quicker tissue destruction, known as rapid progression.
Periodontitis linked to systemic conditions
Certain medical conditions can make gum disease more severe because they affect the body’s ability to respond to inflammation. Uncontrolled diabetes, immune system disorders, and some rare genetic conditions can all contribute to a higher risk of developing periodontitis or experiencing a more rapid progression.
Necrotizing periodontal disease
This is a serious and painful form of gum disease involving the breakdown of gum tissue, ligaments, and bone. It is strongly connected to situations where the immune system is weakened, such as HIV/AIDS, severe malnutrition, high stress, or heavy smoking.
Causes and risk factors for gum disease
Plaque and tartar buildup
Plaque is the primary cause of both gingivitis and periodontitis. If you do not consistently brush your teeth, plaque hardens into tartar. This buildup irritates the gums, leads to inflammation, and increases the risk that gingivitis will progress into a more serious stage of gum disease.
Lifestyle factors: smoking, diabetes, medications
Smoking, uncontrolled diabetes, and certain medications can make it harder to maintain healthy gums. Smoking reduces blood flow to the gum tissue, and diabetes can affect the body’s ability to fight infection. Some medications cause dry mouth, which increases plaque buildup.
Genetics, immune response, and other high-risk factors
Some individuals have genetic tendencies that make them more prone to gum disease. A weakened immune response or chronic inflammation may also raise the likelihood of developing periodontitis.
Periodontitis vs gingivitis treatments
Gingivitis treatment for early-stage gum disease
When we treat gingivitis, our goal is to reduce inflammation and help the gums return to a healthy state. Treatment often includes a dental cleaning that removes plaque and tartar, along with guidance on brushing and flossing. With consistent care, gingivitis usually resolves quickly.
Professional periodontitis treatment options
Periodontitis requires deeper care because the infection is below the gumline. Treatment may involve scaling and root planing, which is a type of professional cleaning that smooths the roots and eliminates bacteria. For more advanced cases, we may recommend follow-up cleanings or additional therapies to stabilize gum health and prevent further damage.
How to prevent gingivitis and periodontitis
Daily gum care routine that actually works
A strong daily routine goes a long way in helping to prevent gum disease. This includes brushing at least twice a day, cleaning between the teeth, and using rinses that support gum health. Consistency is the key to keeping plaque under control.
Professional dental visits and cleanings
Even with great home care, plaque can still harden in areas that are difficult to reach. Regular visits allow us to remove buildup and watch for early signs of trouble. These preventive appointments play a major role in long-term gum health.
Healthy habits that protect your gums long term
Staying hydrated, managing medical conditions, avoiding tobacco, and eating a balanced diet all support strong gums. Small daily choices help protect both the teeth and gums and lower the risk of gum disease progressing.
Need help with gingivitis or periodontitis? Visit Ashley Harrison, DDS
Whether you are noticing early signs of gingivitis or you suspect a more advanced condition, our team is here to help. We provide personalized care, clear education, and treatment plans designed to restore gum health. Early action makes a meaningful difference, and we are committed to supporting patients through every stage of prevention and treatment.
FAQ
What does gingivitis look like?
Gingivitis often shows up as red, swollen gums that bleed when you brush or floss. You may notice a shiny appearance along the gumline or a tenderness that was not there before. In some cases, gingivitis also causes persistent bad breath because bacteria remain around the gums. The gums may feel puffy or irritated, especially after eating or brushing. Since gingivitis is the early stage of gum disease, these changes usually appear before any structural damage occurs. With a cleaning that removes plaque and tartar, along with improved home care, most cases of gingivitis can be reversed.
Is periodontitis reversible?
Periodontitis cannot be reversed once bone loss has occurred, but it can be managed and controlled. The goal of treatment is to stop the disease from progressing and prevent further damage to the gums and supporting bone. Deep cleanings and follow-up care help reduce pocket depth and improve gum health. With consistent home care and regular visits, many patients are able to stabilize their mouths and maintain healthy gums long term. While we cannot replace the bone that has been lost, we can support healthier tissue and reduce inflammation moving forward.
How long until gingivitis turns into periodontitis?
There is no set timeline for how quickly gingivitis progresses into periodontitis. For some individuals, gingivitis may remain stable for months if home care is decent but not ideal. For others, it may progress more quickly due to genetics, medical conditions, or poor oral hygiene. Once plaque hardens into tartar and begins irritating the deeper tissues, the risk of progression increases. The best way to prevent this shift is to treat gingivitis early with a professional cleaning and consistent daily brushing and flossing. Early attention helps stop gum disease before bone loss begins.


